What I Wish my Doctor Knew: Regional Awareness
In a country as developed as the United States, access to healthcare can be taken for granted. This is especially true in affluent suburban regions, like Hamilton County, Indiana, home to suburban communities such as Carmel and Noblesville. According to U.S. News and World Report (2024), Hamilton County stands as not only one of the wealthiest, but also one of the healthiest, scoring a near-perfect score on metrics like economy, education, and public safety. The University of Wisconsin’s County Health Rankings and Roadmaps (2025) consistently places Hamilton County as #1 in Indiana for health outcomes and attributing factors.
By contrast, Scott County, located just 100 miles away in southeast Indiana, consistently ranks among the lowest-performing counties in multiple health indicators. In 2022, the County Health Rankings ranked Scott County 90th out of 92 for health outcomes. Historically, the county has struggled with premature death rates and disease burdens. It was the center of Indiana’s 2015 HIV outbreak, largely driven by opioid misuse and limited access to care (County Health Rankings & Roadmaps, 2025).
These two counties, only a few hours apart, highlight a troubling reality that where you live can profoundly shape how, when, and even if you receive care. The stark difference between Hamilton and Scott County serves as a reminder that healthcare disparities are not just a global issue–they exist right here in Indiana. By examining these regional gaps, this piece aims to bring attention to the urgent need for expanded and sustainable primary care services, greater specialty access, and equitable resource allocation in rural communities that are too often overlooked.
Figure 1
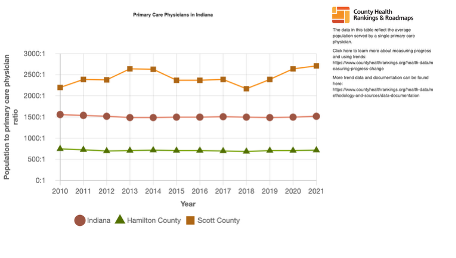
Access to care: Access to primary care physicians (PCPs) and dentists is a foundational element of preventive health and early disease management. Unfortunately, rural counties such as Scott County face significant shortages in healthcare providers compared to suburban areas like Hamilton County.
Figure 1 compares the population-to-primary care physician ratio across Indiana, Hamilton County, and Scott County from 2010 to 2021. Hamilton County consistently maintains a much lower ratio, around 600 to 700 people per primary care physician, reflecting better access. In contrast, Scott County experiences ratios of over 2,000 to 2,700 people per physician. This indicates that residents may have to wait longer or travel further for basic healthcare services. The Indiana state average lies between these two extremes, demonstrating that Scott County shortages are well outside the norm.
A similar situation is evident in the population-to-dentist ratio from 2010 to 2022, with Hamilton County maintaining a relatively low ratio of roughly 1,400 to 1,500 people per dentist, while Scott County’s ratio often exceeds 3,400 people per dentist. This significant difference highlights the limited availability of dental services in rural areas, which can lead to neglected oral health, which is a known risk factor for many systemic diseases (County Health Rankings & Roadmaps, 2025).
Figure 2
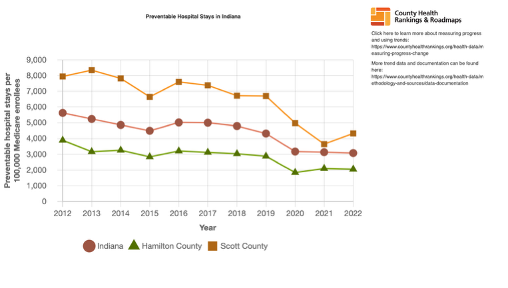
Preventable Illness & Health Outcomes: Health outcomes are deeply intertwined with access to care, and the consequences of provider shortages are evident in metrics such as preventable hospital stays and years of potential life lost (YPLL) due to premature death.
As shown in Figure 2, Scott County exceeds the state average reaching over 8,000 hospital stays per 100,000 Medicare enrollees. This is nearly triple that of Hamilton County. These are hospitalizations that could have been avoided with proper access to routine care, chronic disease management, and follow-up.
Figure 3
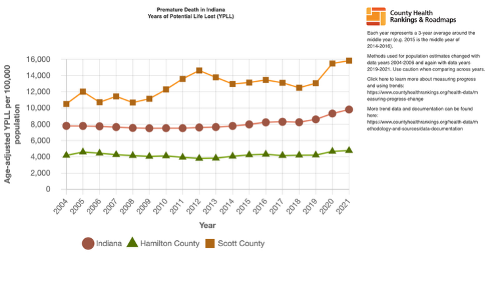
The gap is just as wide when looking at premature death, as seen in Figure 3. YPLL data shows that Scott County has persistently high early death rates, again, nearly triple that of Hamilton County. This rate has continued to climb throughout the years reaching above 15,000 YPLL in 2021 compared to Hamilton County’s 4,000 YPLL.
All of the factors mentioned throughout this paper shape the broader health outcomes of the community. In Scott County, these compounding challenges contribute to a life expectancy of just 69.1 years, which is 6 years below the Indiana state average and an alarming 11.6 years lower than Hamilton County’s (County Health Rankings & Roadmaps, 2025).
Next Steps: Together, these statistics highlight a dangerous cycle of limited access to care leads to unmanaged conditions, which then drive preventable hospital visits and ultimately premature mortality. Where you live can determine how long you live, how easily you can access care, and how often you are forced to go without it. Rural communities like Scott County continue to experience worse outcomes because of a lack of access to primary care, dental care, specialty services, and the infrastructure that supports health.
If we hope to improve outcomes statewide, we must prioritize investment in medically underserved regions. This includes increasing incentives for providers to practice in rural areas, expanding telehealth infrastructure, funding community health programs, and ensuring transportation and preventive services are within reach for everyone, regardless of zip code.
Citations
County Health Rankings & Roadmaps. (2025). Compare counties: Hamilton County, Scott County, and Indiana. University of Wisconsin Population Health Institute. https://www.countyhealthrankings.org/health-data/compare-counties?compareCounties=18000%2C18057%2C18143&year=2025
U.S. News & World Report. (2024, June 8). Healthiest Communities rankings for 2024: Hamilton County, Indiana, ranked #5 of the top 500 healthiest communities. U.S. News & World Report, L.P. https://www.usnews.com/news/health-news/articles/us-news-releases-healthiest-communities-rankings
About the Author
 Christina Schroedle is a second-year osteopathic medical student at Marian University’s College of Osteopathic Medicine. Born and raised in Indianapolis, she is passionate about exploring health disparities within her home state and raising awareness in her community. She is currently interested in pursuing a career in neurology, internal medicine, or family medicine. Outside of medicine, Christina is learning to play golf and training for a marathon. Thank you for taking the time to read!
Christina Schroedle is a second-year osteopathic medical student at Marian University’s College of Osteopathic Medicine. Born and raised in Indianapolis, she is passionate about exploring health disparities within her home state and raising awareness in her community. She is currently interested in pursuing a career in neurology, internal medicine, or family medicine. Outside of medicine, Christina is learning to play golf and training for a marathon. Thank you for taking the time to read!
About Franc Notes
Discover the voices of Marian University's health professions students through "Franc Notes", a vibrant, student-led blog that embodies our Franciscan commitment to community, reflection, and compassionate service. Inspired by the rhythm of "SOAP notes," it features weekly insights—from "DO Diaries" interviews with physicians to summer reflections and program spotlights—fostering collaboration across disciplines."
